Normal Morrison’s Pouch/RUQ
****
This webpage contains:
-
Abdominal Trauma FAST Scans
-
Chest Trauma FAST Scans
-
Trauma FAST Pearls
-
Hemothorax Ultrasound
****
Abdominal Trauma FAST Scan
- Probe & Positioning: Use a curviliear 3.5 MHz or 5 MHz transducer to obtain the images of deeper structures. Start your scan in the mid to posterior axillary line just below the costal margin to avoid rib shadow. After hepatoreanal and splenorenal views, move to the pelvis
- Target Confirmation: Look for dark, anechoic fluid above and below the diaphragm as well as in Morrison’s pouch and the inferior tip of the liver and behind the bladder
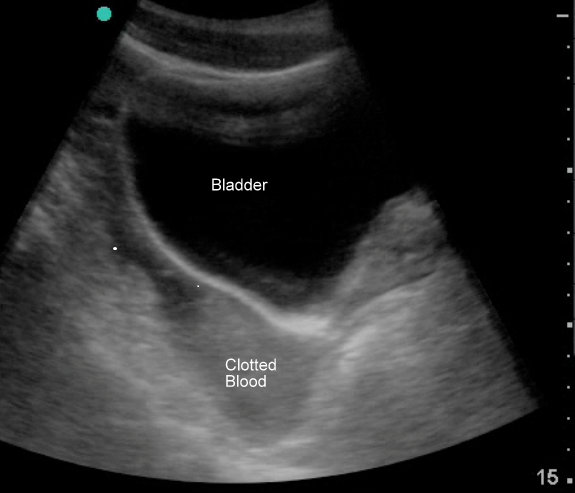
- Blood: Blood appears anechoic (black) when acute and free flowing, but hypoechoic (gray) when subacute or clotted. When blood is gray it is much easier to miss, especially if you are not looking for it. Blood in the pericardial space that is related to trauma is often hypoechoic (gray).
- Rinse & Repeat: The sensitivity of ultrasound in trauma improves with Trendelenberg positioning, repeat imaging and if you know how and where to look (experience). Always image the inferior tip of the liver, as this area may be positive when Morrison’s pouch is not. Also, turn down the gain on the pelvic view if the bladder is full, otherwise the enhancement behind the bladder may “white out” a small pocket of fluid.
- Sensitivity & Specificity: The sensitivity of the FAST scan is ~85% if done serially, but as low as 24% in some studies. Usually >200ml of fluid can be detected. The specificity of the FAST exam is about 95%. False positives may include fluid mimics such as the prostate, psoas, a perinephric fat pad, severe hydronephrosis or a large blood vessel. They may also include other causes of free fluid such as ascites, urine, physiologic fluid, and inflammatory fluid from infection, pancreatitis or ischemic bowel
Get a free subscription to Emergency Physician Monthly
****
Normal LUQ
****
Normal Bladder
****
RUQ View with Free Fluid (Image courtesy of Teresa Wu, MD)
****
Behind the Bladder: Large Free Fluid
****

Fluid in the pouch of Douglas (transverse view)
****
Chest Trauma FAST Scan
- Probe & Positioning: Use a curviliear 3.5 MHz or 5 MHz transducer to obtain the images of deeper structures. Scan at the left parasternal border, subxyphoid and at bilateral costal margins in the mid-axillary line
- Target Confirmation: Look for dark, anechoic fluid above and below the diaphragm as well as in around the heart.
- The Heart: If you cannot see the heart at all on the parasternal view, consider a small anterior left sided pneumothorax until proven otherwise. The chest film usually will not be sensitive enough to pick this up. If the patient is going to the OR consider either going to chest CT first or placing an empiric chest tube if the patient remains unstable and must be rushed to surgery. Blood appears anechoic (black) when acute and free flowing, but hypoechoic (gray) when subacute or clotted. When blood is gray it is much easier to miss, especially if you are not looking for it. Blood in the pericardial space that is related to trauma is often hypoechoic (gray).
- The Lungs: Ultrasound can also be used to evaluated directly for pneumothorax or hemothorax. For hemothorax use the curvilinear probe to image above the diaphragm for fluid. Ultrasound is more sensitive than x-ray as it can detect as little as 20ml of fluid. For pneumothorax, use the linear small-parts probe in the sagittal plain. If safe, elevate the head of the bed 60 degrees and scan 2-3 interspaces at the most anterior part of chest. Look for the absence of the normal lung sling & comet tail artifacts that move with respiration. Sensitivity has been reported at ~95%, which is better than chest x-ray. False positives include mainstem intubation, bleb, infiltrate, contusion, ARDS, atelectasis, adhesion, and pulmonary fibrosis

Non-traumatic effusions are more likely to be black than gray.
****

Normal sub-xiphoid cardiac view.
****

Small left Pneumothorax seen on CT but not seen on CXR. With ultrasound you won’t be able to find a window to the heart on the parasternal view, but will instead get “reverb” artifact.
****
Trauma FAST Pearls:
- Older Blood is Gray: Blood appears anechoic (black) when acute and free flowing, but hypoechoic (gray) when subacute or clotted. When blood is gray it is much easier to miss, especially if you are not looking for it. Blood in the pericardial space that is related to trauma is often gray even when acute. See images below
- Check the Liver Tip: Sometimes if there is only small amount of hemoperitoneum it will only be seen at the inferior anterior liver tip. See image below.
****

Clotted blood within the urinary bladder from a GSW
****

Fluid seen nowhere else but at the inferior anterior tip of the liver. Morrison’s view was negative on this patient.
****

GSW Traumatic Tamponade: blood of intermediate density
****

GSW Traumatic Tamponade: blood is often close to liver density
****
Ultrasound Detection of a Hemothorax by Teresa Wu, MD
-
The traditional four-view FAST exam can be expanded to evaluate the pleural space just cephalad to the bright hyperechoic hemidiaphragm.
-
Because trauma patients are often lying supine strapped to a backboard in cervical spine precautions, portable chest radiographs may not detect small hemothoraces.Bedside ultrasound can be used to quickly assess for the presence of a hemothorax, and is often better than chest radiography in detecting small amounts of pleural fluid (sensitivity 94.6-97% and specificity 99-100%).
-
Use the curved array 2.5 to 3.5 MHz transducer or phased array transducer on most patients.Lower frequency probes provide greater penetration in patients with an obese body habitus.
-
Ensure consistent image directionality by orienting the external identification dot of the transducer towards the patient’s right or towards the patient’s head.The indicator dot on the screen should be to the right of the ultrasound image.
-
Position the probe in an oblique angle in the mid-axillary line between the 8th and 11th ribs.Once you identify the hyperechoic bright white diaphragm, angle the ultrasound beam more cephalad to evaluate the pleural space just above the diaphragm.
-
Normal lung tissue in the dependent areas of the thorax will share approximately the same echogenicity as a normal liver on ultrasound.Free fluid in the pleural space will appear as a dark anechoic stripe just cephalad to the diaphragm.
-
Observe the pleural space through a full respiratory cycle to monitor changes and characteristics of the fluid with diaphragm movement.Use the sonographic images to help localize the ideal interspace for chest tube insertion.
-
Remember that blood will appear less anechoic and more hypoechoic (gray rather than black) as it clots.Do not mistake clotting blood in the pleural space for normal lung tissue.Scan cephalad above the clot to search for the more hyperechoic lung tissue floating within the hemothorax.
Hemothorax – Image courtesy of Teresa Wu, MD
****
Do you want a pocket reference that has essential material on ED Ultrasound as well as other imaging, labs, EKG’s, procedures, risk management and more?
Then get the Tarascon Emergency Department Quick Reference Guide, 2nd edition
****
WOULD YOU LIKE TO USE ONE OF OUR IMAGES?
As long as you paste the following statement with a weblink to this site, no problem: “Image reproduced with permission, ERPocketBooks.com”
****