History of Present Illness:
A man in his mid-40’s presents to the hospital with a first time seizure. He recovered from covid 2 weeks ago, but has been having a frontal headache for the past week associated with vomiting and 5-10 lb. weight loss. His doctor gave him amoxicillin and tramadol for possible sinusitis, which he started 3 days ago. Last night he noted tremor in his left arm. EMS notes wife heard him groan then witnessed about 30 sec of generalized tonic clonic seizure. When EMS arrived he was postictal but now he is alert and coherent. He denies any fever, neck stiffness, visual changes, focal weakness, slurred speech, loss of sensation or ataxia. He also denies any cp/sob or palpitations prior to loss of consciousness.
Vital Signs & Physical Exam:
Awake and alert x 4, conversational, no slurred speech, no facial droop, 5/5 strength throughout, normal sensory throughout, left upper extremity tremor present on testing finger to nose testing but no tremor noted on pronator drift testing. no evidence of truncal ataxia.
Initial Diagnostic Testing:
- CBC: normal except for hemoconcentration
- Chem-7: normal except for k = 3.0
- Imaging:
What is the most likely diagnosis?
- A) medication induced seizure
- B) subdural hematoma
- C) cerebral venous thrombosis
- D) cerebral emboli
SCROLL DOWN FOR ANSWERS & 1-MINUTE CONSULT
<<<<<<<<<<<<<<<<<<<<< ADVERTISEMENT & SPACER >>>>>>>>>>>>>>>>>>>>>
****************************************************************************
THE EMERGENCY MEDICINE POCKETBOOK TRIFECTA
Get one of our publications, all designed specifically for Emergency Care Providers
Emergency Medicine 1-Minute Consult, 5th edition
A-to-Z EM Pharmacopoeia & Antibiotic Guide, 5th edition, BRAND NEW
8-in-1 Emergency Department Quick Reference, 5th edition, NEW
******************************************************************************
***************************************************************************
<<<<<<<<<<<<<<<<<<<<<<<<< END SPACER >>>>>>>>>>>>>>>>>>>>>>>>>
ANSWER:
- A) medication induced seizure – good thought as penicillins can cause seizure
- B) subdural hematoma
- C) cerebral venous thrombosis – CORRECT – see below
- D) cerebral emboli
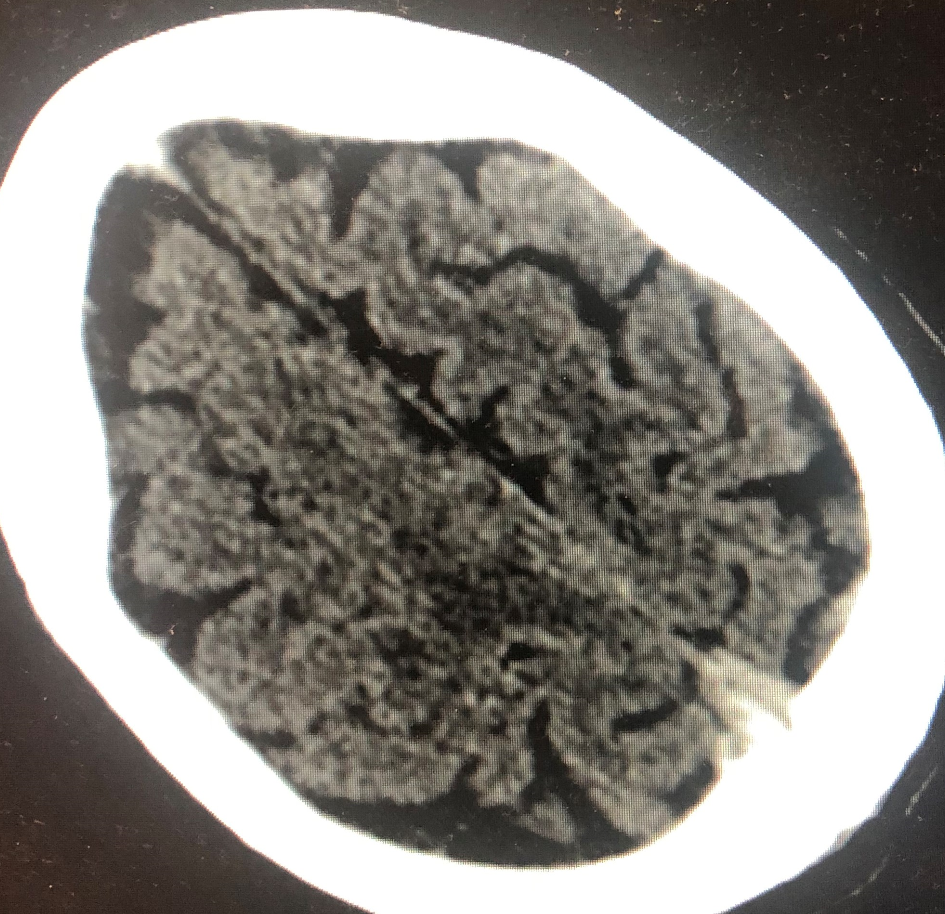
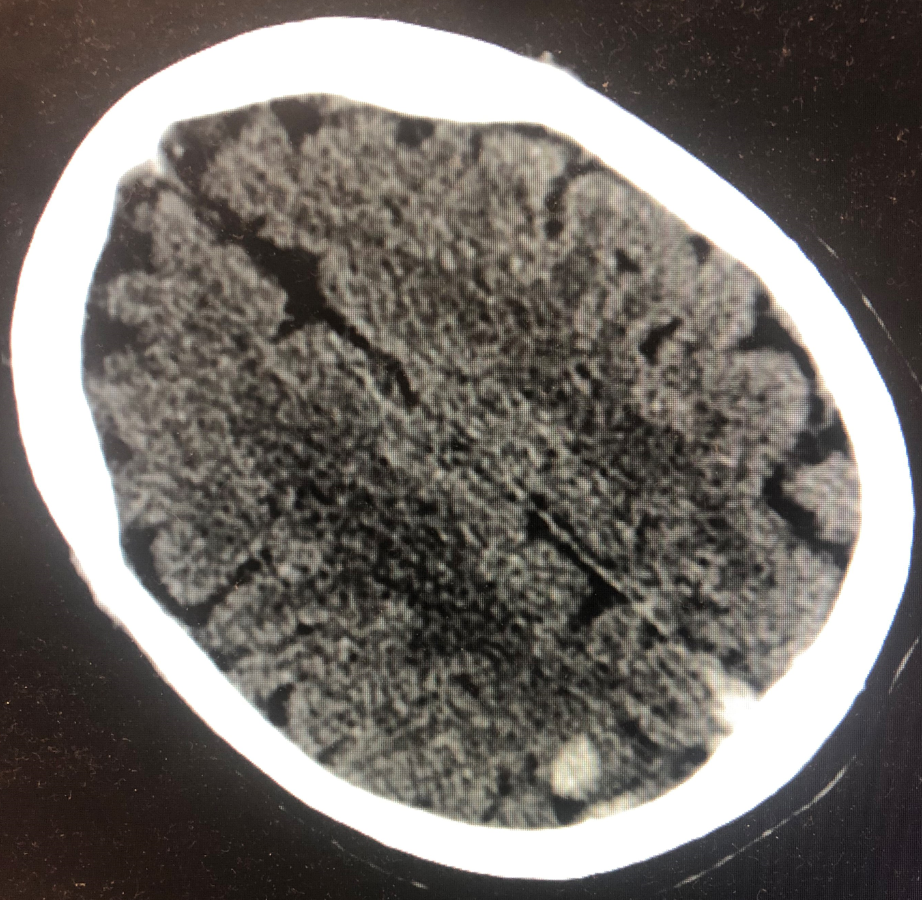
CT above shows increased density and enlargement of the dural venous sinus concerning for cerebral venous thrombosis (CVT). Another cut, shown below, shows an 11 mm parenchymal hemorrhage in the posterior right parietal lobe that is likely a hemorrhagic venous infarct, a known complication of CVT
1-Minute Consult on this topic: Click HERE and scroll to the TOP of page 176.
CASE CONCLUSION: CT venogram confirmed the diagnosis. It was thought to be a post covid complication. He had not received any recent vaccines. Despite the hemorrhagic conversion, he was started on heparin at the lower cardiac dose, after neurology consultation of course.
