Normal Uterus in Transverse
****
This webpage contains:
-
Pelvic Ultrasound: Early Pregnancy
-
Pelvic Ultrasound: Late Pregnancy
-
Pelvic Ultrasound: Not Pregnant
****
Pelvic Ultrasound: Early Pregnancy:
- Assess Stability: Try to avoid sending a potentially unstable patient to radiology. If you have the skills, perform a bedside ultrasound yourself and call your surgeon early. If not, have your ultrasound tech come to the ED to scan at the bedside.
- Basics: The EM physician rarely needs to do a trans-vaginal scan. With a trans-abdominal you can usually tell if there is an IUP or not (to rule out ectopic), and if there is free fluid or not (to rule out rupture). This, and evaluation for cardiac motion should be the extent of a limited bedside ultrasound. The order of appearance of structures within the uterus in pregnancy a gestational sac (beware of pseudosacs) then a yolk sac, then a fetal pole, then finally cardiac motion.
- Free Fluid: Free fluid in the pelvis or abdomen should be considered blood until proven otherwise. Blood and ascitic fluid may look the same on ultrasound. In the proper clinical scenario, such a hemodynamically stable patient with no history of trauma and a benign exam, ascites may be considered. Other causes of free fluid may include pus or bowel or bladder rupture.
- Start at Morison’s: Begin by scanning the hepatorenal recess (Morison’s pouch). This is the most dependent position in a supine patient so free fluid may collect here. If you see fluid here, call for help ASAP. Any patient with a positive pregnancy test and free fluid visible on bedside ultrasound should be suspected of having a RUPTURED ectopic pregnancy until proven otherwise.
- The Pelvis: After Morrison’s pouch evaluate the pelvis. This is the most dependent part of the abdomen when upright. To get the best views, the patient should ideally have a full bladder to serve as an acoustic window. If she just gave a urine sample, you will have to do your best. Look for hypoechoic free fluid in the vesicouterine and rectouterine spaces and assess the uterus for the presence or absence of an IUP. In a ruptured ectopic all you may see is a confusing mess of heterogeneous clotted blood that can even make it hard to delineate the uterus. If you have done plenty of scans of the normal pelvis, which you should have, you will be able to tell that “something looks wrong” though you may have a hard time accurately determining exactly what you are looking at. (For transvaginal scanning see the final section on this webpage).
- Beware: A cornual ectopic, which is the most dangerous type of ectopic due to rich blood supply to the cornua, can be close enough to the uterus to fool you into thinking it’s an IUP if you are not careful. Make sure there is at least a 2 cm mantle of myometrium on all sides of a gestational sac before diagnosing and IUP. Also beware of pseudosacs, irregular intrauterine sacs that can co-occur with an ectopic.
Want more educational images? Check out the ED Atlas on CD
****
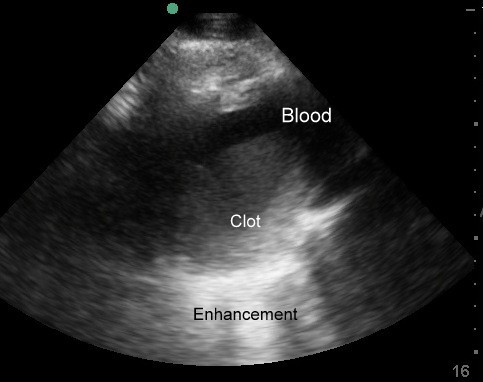
Ectopic Pregnancy with clot around uterus
****
****
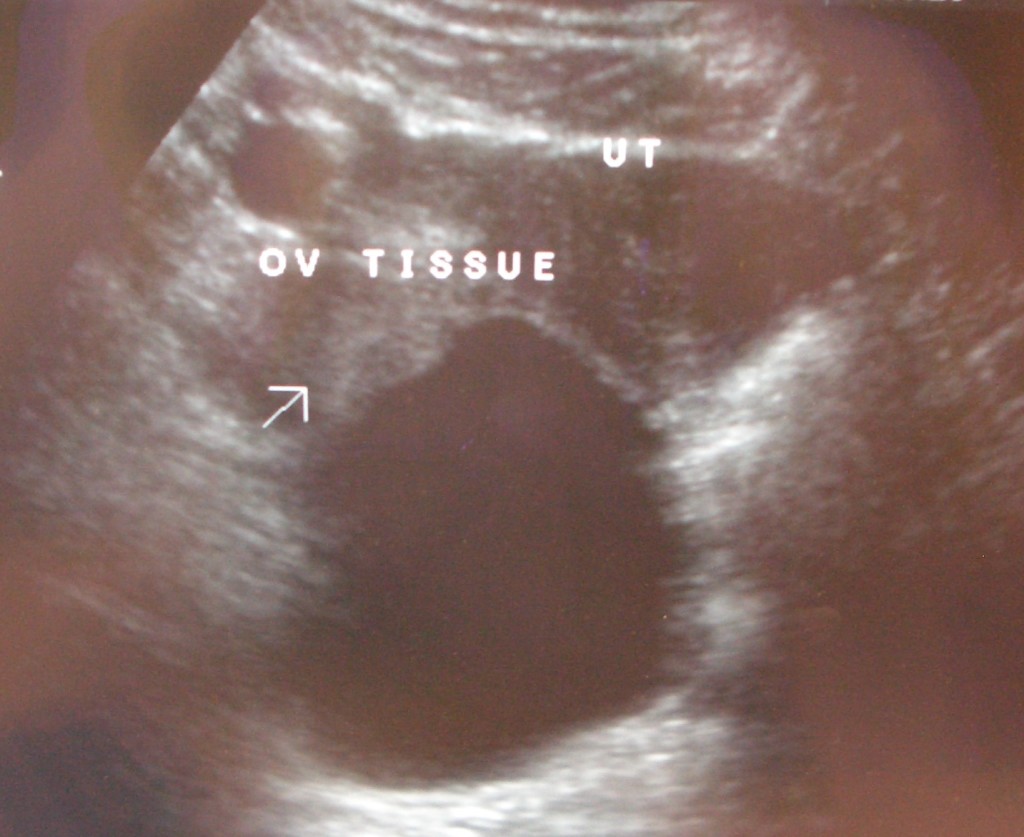
Cornual Ectopic Pregnancy. Mid-uterus is empty. Sac is in the right horn of the uterus
****
Cornual Ectopic Pregnancy. If your not careful, this can look like an IUP
****
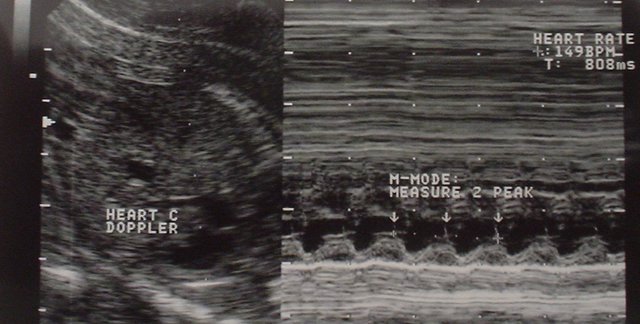
Using B/M mode split screen to measure Fetal Heart Rate
****
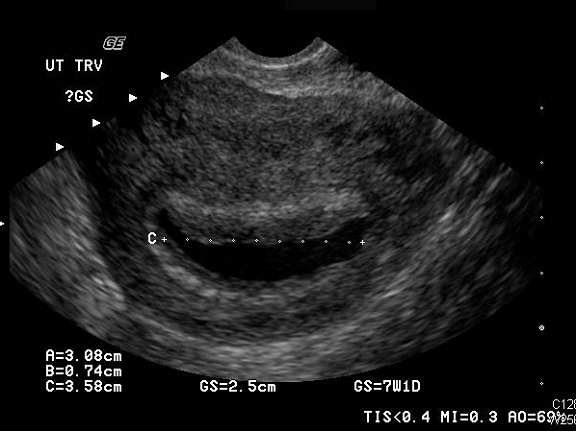
Pseudosac in a patient with Ectopic Pregnancy (Courtesy of Julie Vajnar, PA-C)
***

Ruptured ectopic with free fluid in pouch of Douglas
*

Hydatidiform Mole
****
****
Pelvic Ultrasound: Late Pregnancy
come back later
****
Pelvic Ultrasound: Not Pregnant:
- Basics: Although transvaginal ultrasound is more sensitive than transabdominal ultrasound for the evaluation of the female reproductive organs, the ED physician rarely needs to perform a trans-vaginal scan. With a trans-abdominal you can usually tell if there is any pathology that requires emergent treatment, such as a huge cyst that could torse an ovary, a big abscess, or other major condition. When there is concern for a less emergent condition such as a routine ovarian cyst, a formal ultrasound should be ordered.
- Free Fluid: Fluid tends to accumulate between the bladder, which will always be anterior, and the uterus. Very small amounts of free fluid soon after ovulation may be physiologic, but would rarely be noted on a trans-abdominal ultrasound. Larger amounts of fluid may have the appearance of cat ears, or if a bit larger may look like a bow-tie. Rarely hemorrhagic cysts in non-pregnant patients can cause massive internal bleeding. If there is a large amount of free fluid, emergency surgery could be indicated, especially if it tracks into Morrison’s pouch, even if the pregnancy test is negative.
- The Uterus: The normal uterine dimensions in a woman of reproductive age is about 7.5 cm long, 4.5 cm wide and 3.0 cm thick. It would usually be smaller during premenarche or menopause.
- The Endometrium: The normal endometrial stripe thickness varies but usually is <15 mm during the reproductive years and <5 mm during menopause. Thickness can change depending on the phase of the menstrual cycle or, during menopause, on the use hormonal therapy or Tamoxifen. After an abortion the thickness should be <5 mm.
- The Ovaries: Normal ovaries in a woman of childbearing are usually 3-5 cm in length. Simple cysts under 2.5 cm in diameter are often painless but complex or hemorrhagic ovarian cysts that are smaller or simple cysts that are larger than 2.5 cm often do cause pain. Pain from an ovarian cyst usually starts mid-cycle and usually ends by menses. Cysts between 5-10 cm are highest risk for ovarian torsion. Cysts smaller than 5 cm and those larger than 10 cm are less likely to torse. In infection, tubo-ovarian abscesses (TOA) may occur.
- Practice, Practice, Practice: Whenever you scan for alternate indications in a women, practice looking at the pelvis with trans-abdominal ultrasound. The more normal patients you look at, the more likely you are to recognize when something is not right. With bedside ultrasound there is no substitute for experience. The more ultrasounds you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is.

Tubo Ovarian Abscess read more about this case
****
2 months of backed up blood and clot from Uterine Cervical Stenosis after multiple D & C s
****
Ovarian Torsion from large ovarian cyst in 15 year old girl
****
TRANS-VAGINAL:
- Basics: Usually these are formal, radiology performed studies, but they can be performed in the ED if you are set up for it. Make sure you have a chaperone. To make trans-vaginal ultrasound less painful, let the patient put the probe in her vagina herself. Make sure you have a chaperone.
- Weeks: Here’s is what you should see on transvaginal ultrasound depending on the number of weeks gestation: 5-6wks: Sac 6-7wks: Pole & Cardiac Motion.
- Precautions: Avoid trans-vaginal imaging if the patient had a recent gynecologic procedure. Ultrasound is only 40% sensitive for placental abruption
- Flow: Always assess for vascular flow to ovaries in order to rule-out ovarian torsion.If adequate images are not able to be obtained via the transabdominal approach, a transvaginal ultrasound can be performed at the bedside. Cover the endovaginal transducer with a gel filled sheath and apply a copious amount of sterile gel to the outside of the sheath. Insert and advance the transducer with the indicator marker pointing anteriorly towards the patient’s pubic symphysis. Alternatively, you may let the patient insert the probe herself as this method is often less uncomfortable. Scan through the uterus in this sagital plane, noting the presence or absence of an intrauterine pregnancy.
- Optional – Look for the Ectopic: It is often possible to visualize the ectopic pregnancy during a quick transvaginal bedside scan. Rotate the probe 90° counter-clockwise and point the indicator marker towards the patient’s right side. Trace the broad ligament of the uterus out towards the ovaries, which lie just medial to the iliac vessels. Look for any complex adnexal masses or tubal rings.
****
Do you want a pocket reference that has essential material on ED Ultrasound as well as other imaging, labs, EKG’s, procedures, risk management and more?
Then get the Tarascon Emergency Department Quick Reference Guide

****
WOULD YOU LIKE TO USE ONE OF OUR IMAGES?
As long as you paste the following statement with a weblink to this site, no problem: “Image reproduced with permission, ERPocketBooks.com”
****