History:
A man in his early-60’s presents to the hospital with 1 day of pleuritic central chest pressure. He had an MI with a stent about 3 weeks ago but was told there were two other arteries with 20% and 50% narrowing that were going to be treated medically without stenting.
Exam:
Vital signs are normal except for lowish BP. Physical exam is normal otherwise.
An ECG is done
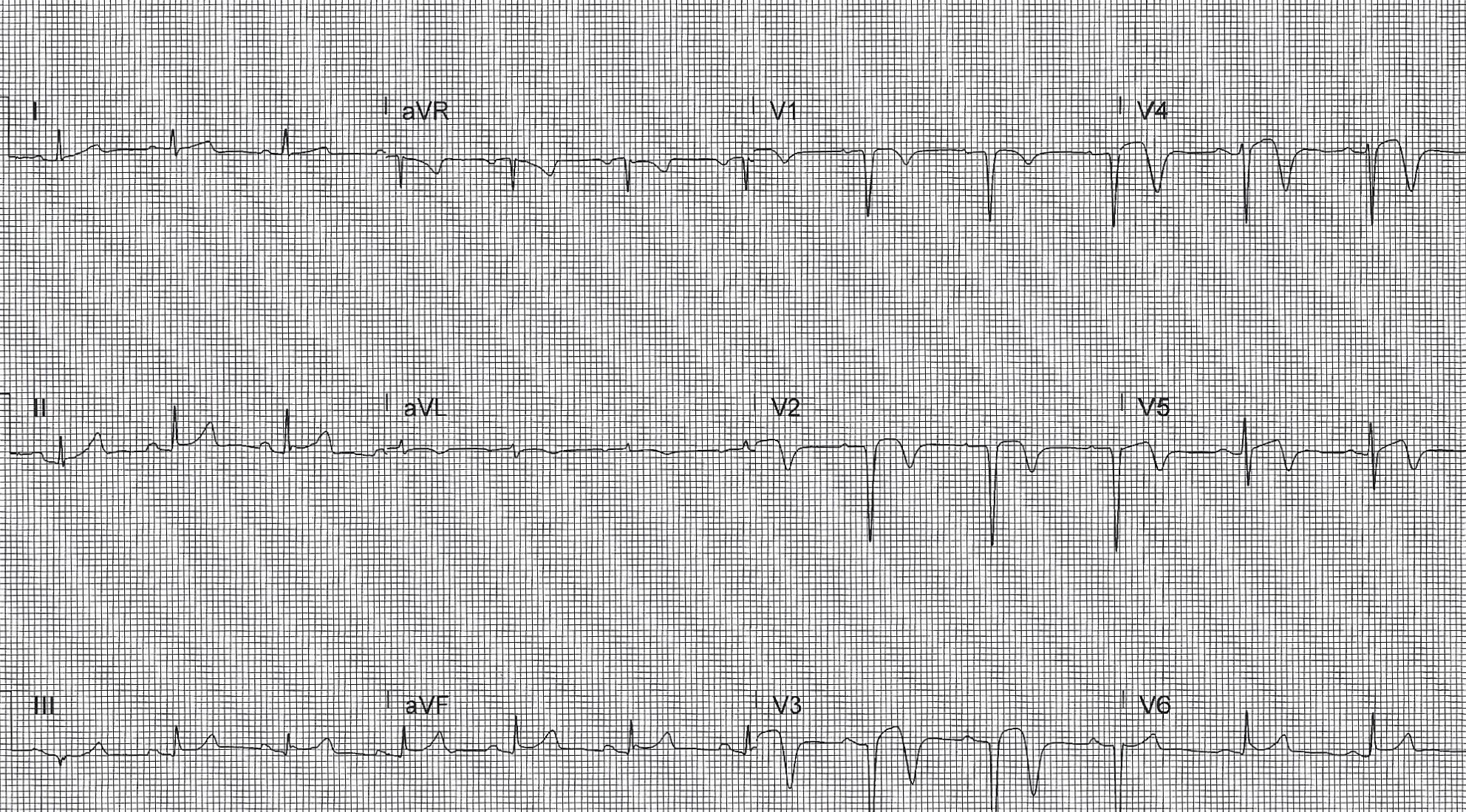
Computer Read: NSR at 74, anteroseptal MI, probably recent
What is the most cause of EKG findings in this patient?
- A) MI
- B) pericarditis
- C) PE
- D) GERD
SCROLL DOWN FOR THE EKG ANALYSIS & 1-MINUTE CONSULT
<<<<<<<<<<<<<<<<<<<<< ADVERTISEMENT & SPACER >>>>>>>>>>>>>>>>>>>>>
THE EMERGENCY MEDICINE POCKETBOOK TRIFECTA
Emergency Medicine 1-Minute Consult, 5th edition
A-to-Z EM Pharmacopoeia & Antibiotic Guide, NEW 5th edition
8-in-1 Emergency Department Quick Reference, 5th edition
******************************************************************************
<<<<<<<<<<<<<<<<<<<<<<<<< END SPACER >>>>>>>>>>>>>>>>>>>>>>>>>
ECG ANALYSIS, QUIZ ANSWER, CASE OUTCOME/PEARLS & 1-MINUTE CONSULT:
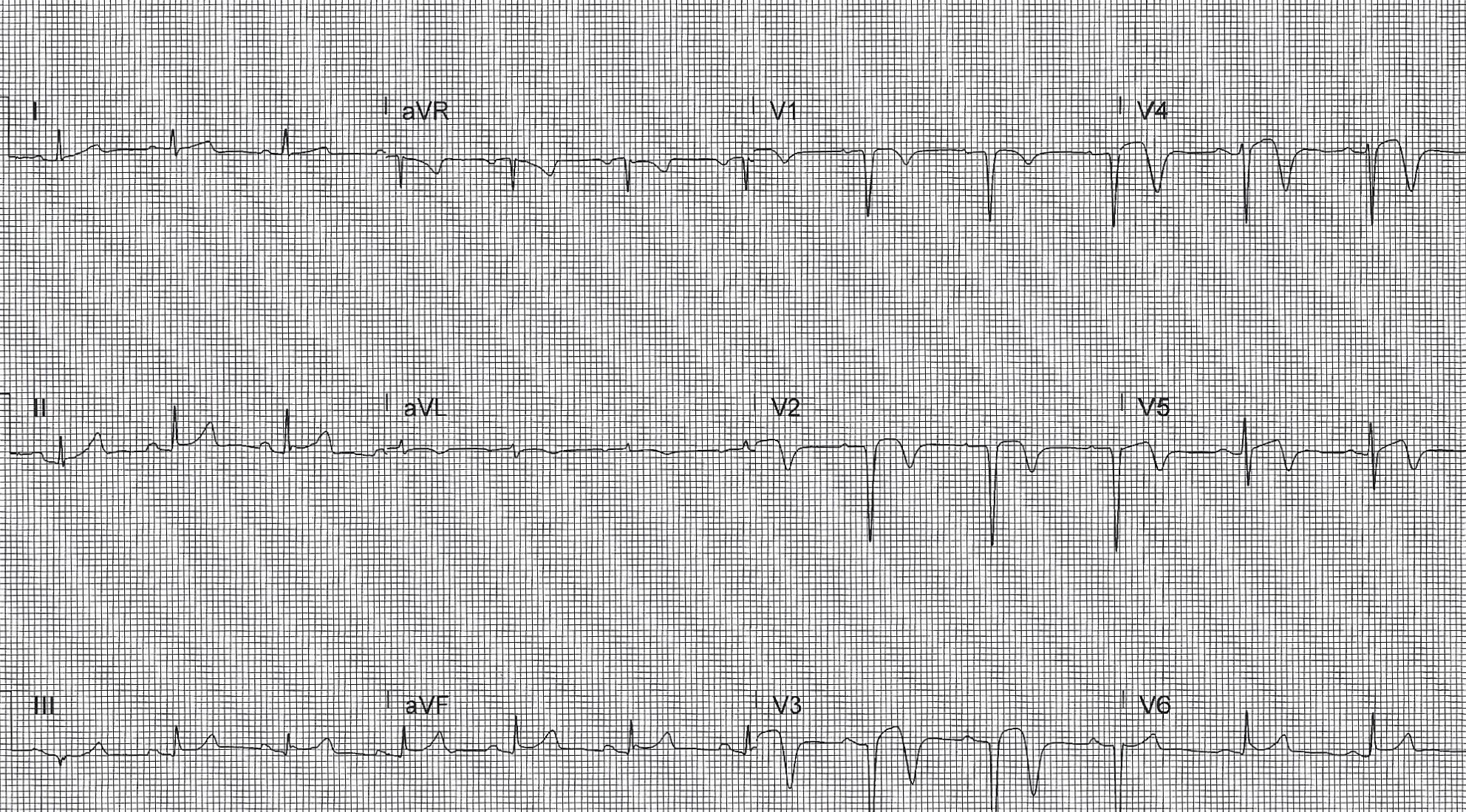
My ECG interpretation (by Dr. D. Brady Pregerson of ERpocketbooks.com): There is diffuse ST elevation in the anterior leads more that inferior and lateral. There is PR depression best seen in the inferior and lateral leads. There are biphasic T waves in the precordial leads that look like reperfusion T-waves. This EKG could be consistent with pericarditis, reperfusion from a STEMI or STEMI on top of abnormal T-waves. Since the patient is having active chest pain and has known CAD it is safest to assume STEMI until proven otherwise because treatment of an occlude artery is the most emergent.
What is the most cause of EKG findings in this patient?
- A) MI – Correct first impression. There are reperfusion T-waves but still some ST elevation, which could be new and represent new ischemia. He went to cath
- B) pericarditis – CORRECT final impression. Dressler’s syndrome became the most likely diagnosis once MI was ruled out.
- C) PE – good thought with pleuritic pain
- D) GERD – unlikely here. Also a diagnosis of exclusion
Outcome: went to cath, which was negative. Troponin was negative. Developed low grade fevers but no leukocytosis or pleural effusion. Diagnosed with Dressler’s syndrome
Emergency Medicine 1-Minute Consult:
Dressler’s: AKA Post-myocardial infarction syndrome: rare autoimmune process in <5% of MI’s
Clinical: Onset 1-12 weeks post MI: fever, leukocytosis, pericarditis >pleural effusion, pleuritis
Causes: MI >cardiac surgery, chest trauma, electrophysiology procedures, other insults to the heart
Treatment: Short course of steroids or non-aspirin NSAID
***
