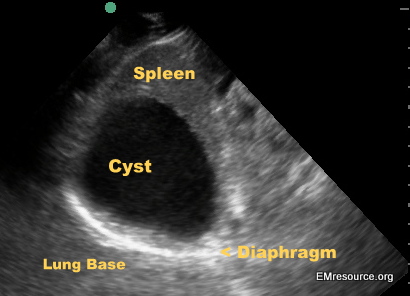
Normal LUQ Sonogram
****
Left-Upper Quadrant Ultrasound
- Left Flank Window: From the left flank you should be able to see the left lung base, diaphragm, spleen and left kidney. If rib shadow is obstructing the view have the patient breath in and hold their breath to move the spleen and kidney lower.
- Epigastric Window: The muscular lining of the stomach will appear as a bright white, hyperechoic lining surrounding a dark black, anechoic gastric lumen just to left of midline in the left upper quadrant. It can be viewed to asses for gastric distension and to confirm G-tube placement (see below). The pancreas can also be viewed from this window but may be obstructed by gas. Imaging of the pancreas is not usually performed by an emergency physician.
****
Case: An elderly female presents to the ED with RUQ pain and vomiting
On exam she is hypotensive and had diffuse right sided abdominal and epigastric tenderness.
You perform a bedside US to look at the gallbladder and the aorta. The image you obtain is shown below.
What is going on here?
Intraperitoneal Free Air on Ultrasound
- Large Free Air Causes Reverb Artifact: Reverberation artifact, repeating bands of white and dark from reflection of the ultrasound beam back and forth between the probe and the peritoneal stripe, occurs at a large tissue/air interface. It’s kind of like the repeated reflection of yourself that you would see if you were standing between two parallel mirrors. The best place to look for this is epigastric or RUQ. The significance of this is that there is a lot of air blocking your view. With this degree of artifact continuing to look for the aorta will likely prove difficult or fruitless. You should instead immediately assume that the patient has a perforated viscus causing free air to leak into the peritoneal cavity. Sensitivity may be increased with the head of bed elevated to 10-20 degrees. Note that a large collection of intraluminal air close to the surface can also cause reverb artifact and thus mimic free air.
- Small Air Bubbles Cause Echogenic Foci with Comet Tail Artifact: This may be best seen withing ascitic fluid or between the right hemidiaphragm and the liver. Sensitivity can be increased by turning the patient into the left lateral decubitus position with the head of bed slightly elevated so that air bubbles rise to the right side above the liver. Normal air pockets within the intestinal lumen should move with bowel peristalsis.
- Consider Switching to the Linear Probe: When imaging the abdomen one usually uses the curvilinear probe. When free air is suspected, switching to a linear probe may improve resolution as air will usually rise to the near field in the supine patient.
- Pneumoretroperitoneum: If perforation occurs in retroperitoneal structures one may see air around the duodenum, head of the pancreas, or around the kidney. In addition, retroperitoneal vessels (aorta and IVC) may be difficult to visualize.
References:
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3214511/
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3711723/
Normal LUQ
****
****
Confirming G-tube Placement Via Ultrasound
- Old School: Traditional methods used to confirm proper G-tube placement, such as contrast-enhanced KUB, pH testing of gastric aspirate, etc. can be time consuming and are not always 100% sensitive or specific.
- New School: Bedside ultrasound can be utilized to visualize the gastric lumen in a quick, non-invasive manner, without exposing your patient to radiation. Using ultrasound to confirm gastrostomy tube (G-tube) placement is still a relatively new concept, but recent literature supports its high sensitivity and accuracy.
- Orienting: Scan along the patient’s left upper quadrant and identify surrounding structures such as bowel loops, the spleen and diaphragm. The muscular lining of the stomach will appear as a bright white, hyperechoic lining surrounding a dark black, anechoic gastric lumen just to left of midline in the left upper quadrant.
- Viewing the Stomach: Apply sterile acoustic gel near the stoma. Higher frequency probes can be used to visualize superficial structures in thin patients. Lower frequency probes will enable better visualization of internal structures in patients with more subcutaneous fat and muscle. Scan through the entire stomach and obtain longitudinal, sagittal, and oblique views of the entire organ. If the stomach is filled with gastric contents, you will note swirling movements in real-time imaging during peristaltic mixing periods. Some higher frequency probes may enable you to visualize the irregular rugae of the stomach wall.
- Viewing the G-tube: Attempt to visualize the tip of the inserted G-tube or the inflated anchoring balloon within the lumen of the stomach. These structures will appear as white, hyperechoic structures projecting into the hypoechoic stomach cavity. If you opted to fill the G-tube balloon with normal saline, it will appear more hypoechoic than an air-filled balloon.
- Viewing the Jet: Increase the depth of your scan so you can visualize the entire stomach. Inject a small amount of agitated normal saline through the G-tube and watch in real-time as the saline bubbles swirl within the lumen of the stomach.
- Practice: During every abdominal scan, practice viewing the stomach on different patients so you learn how to recognize the subtleties of bedside gastric scanning.
****


PICTURES OF NORMAL GASTRIC SCANNING NEEDED ….
Thank you very very very very very very muchhhhhhhhhhhhhhhhhh