History of Present Illness:
A 72-year-old female with a history of cataract surgery, macular degeneration, HTN and atrial fibrillation presents to the ED for 3 days of decreased vision in her left eye associate with nausea and pain behind her eye. She vomited once on route here. She denies any head trauma, fall, neck or back pain, shortness of breath or other complaints.
Vital Signs & Physical Exam:
Vital signs are normal. Physical exam is normal except for a red eye without discharge and no light perception vision in the left eye. Eye pressure is 61 on the left and 15 on the right
Relevant Test Results:
- EKG: atrial fib, rate controlled
- Labs: none ordered
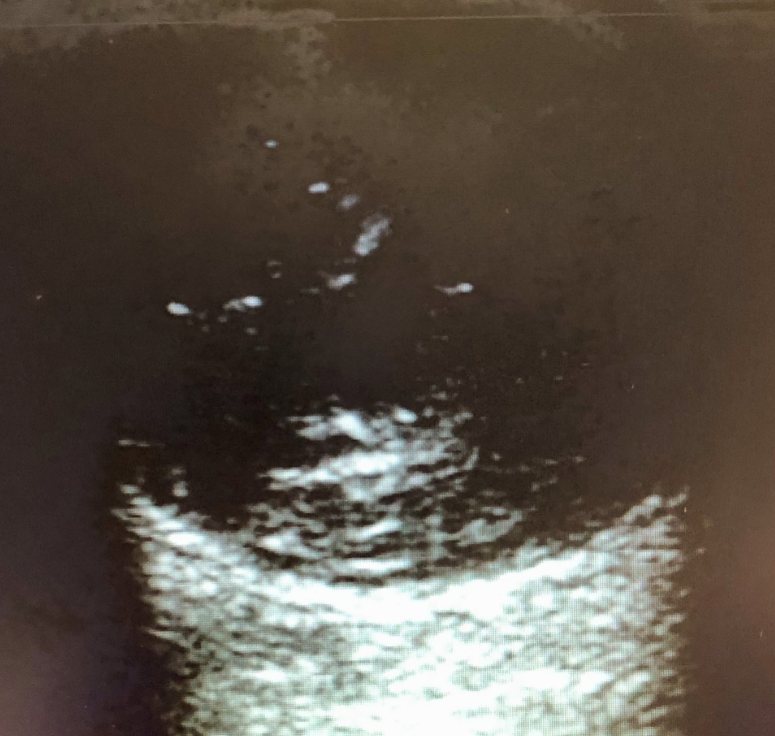
- Imaging: see bedside US below.
What is the most likely cause of the pain?
- A) Glaucoma
- B) Vitreous hemorrhage
- C) Retinal detachment
- D) Central retinal artery occlusion
<<<<<<<<<<<<<<<<<<<<< ADVERTISEMENT & SPACER >>>>>>>>>>>>>>>>>>>>>
THE EMERGENCY MEDICINE POCKETBOOK TRIFECTA
Emergency Medicine 1-Minute Consult, 5th edition
A-to-Z EM Pharmacopoeia & Antibiotic Guide, NEW 5th edition
8-in-1 Emergency Department Quick Reference, 5th edition
******************************************************************************
<<<<<<<<<<<<<<<<<<<<<<<<< END SPACER >>>>>>>>>>>>>>>>>>>>>>>>>
ANSWER: What is the most likely cause of the pain?
- A) Glaucoma – doesn’t show up on imaging
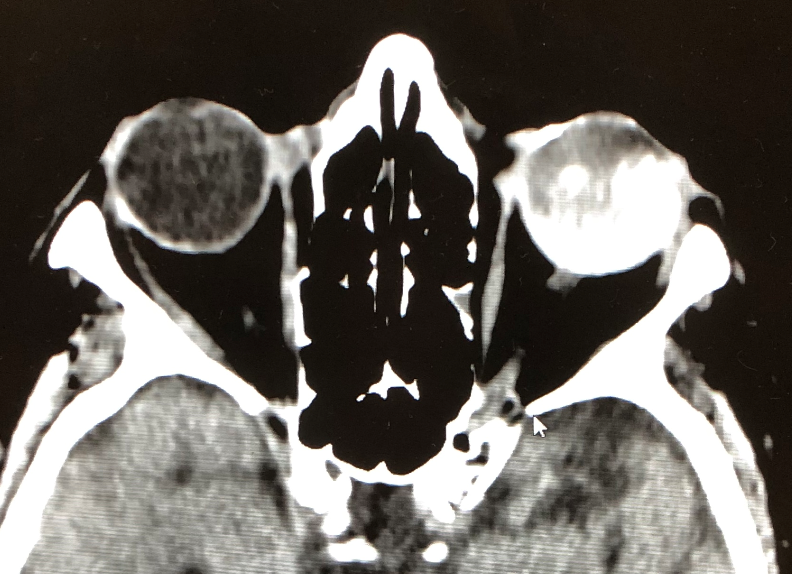
- B) Vitreous hemorrhage – CORRECT – Start glaucoma meds, consider reversing Eliquis. Consult Ophtho. See CT below
- C) Retinal detachment – typically painless
- D) Central retinal artery occlusion – typically painless
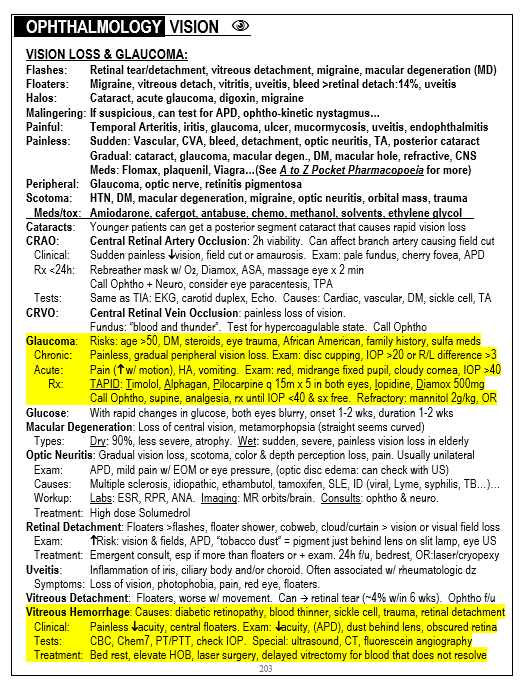
1-Minute EM Consult on the topic for this case from the Emergency Medicine 1-minute Consult Pocketbook
CLICK HERE TO LEAR MORE ABOUT THIS BOOK
CASE CONCLUSION: FFP given. Given the duration of symptoms it was thought unlikely that the eye would recover so no PCC given due to higher risk of stroke nor mannitol given due to higher risk of intracranial bleed. Pressure did not improve for hours. Permanent vision loss from prolonged glaucoma caused by intraocular bleed.
CASE LESSONS:
- Always consider intraocular bleeding in a patient on thinners
- Always consider glaucoma with eye pain, vomiting or vision loss