Closed loop SBO
Acute Appendicitis
****
This webpage contains info on…
-
Bowel Obstruction
-
Appendicitis
-
Intussusception
****
SBO PEARLS & PITFALLS:
- Benefits: Fast, bedside, repeatable, no radiation
- Accuracy: Sensitivity/Specificity below
- XR: 80%/75%: bowel >3cm wide, air-fluid levels, airless, no rectal air [fluid poorly seen]
- US: 85%/85%: bowel >2.5cm that is filled with fluid [air poorly seen]
- CT: 95%/99%: IV contrast helps show ischemia, PO contrast detrimental
- Bowel Obstruction: Dilated loops of bowel will measure >2.5 cm in diameter and contain anechoic (black) fluid within their lumen. Gas-filled bowel may be difficult to visualize with US and will cause scatter over far-field structures.
- Pseudo-mass: A loop of bowel may occasionally look like a mass. The duodenum may look like a solid mass just behind and below the gallbladder and may even produce acoustic shadowing.
- Peristalsis: If you keep your probe steady, you may be able to see the bowel peristalsing. This may help you to identify certain structures as bowel.

Small Bowel Obstruction (lumen is black). If bowel if filled with fluid
****
Small Bowel Obstruction (lumen is black). If bowel if filled with fluid
****
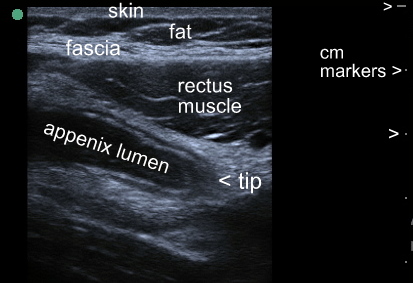
APPENDIX ULTRASOUND:
- Benefits of Ultrasound: avoids both radiation and IV contrast and their small, but real, associated risks. In addition, ultrasound may be faster than CT as there is no need to wait for BUN & creatinine results or for oral contrast to move distally. If you do it yourself it is even faster!
- Sensitivity & Specificity: Both the sensitivity & specificity of ultrasound for appendicitis are less than that of CT. In
- US-Peds: 88% and 94%
- US-Adults: 83% and 93%.
- CT scan: 94% and 95%.
- The accuracy of ultrasound can be worse in overweight patients or those with overlying bowel gas. In addition if the appendix is retrocecal or is lying in a difficult anatomical plane, the study will be more challenging.
- Patient Selection: Ultrasound is an excellent initial imaging modality for the appendix in thin individuals, especially children and young adults. In the pregnant patient, ultrasound is the initial study of choice to evaluate right-lower-quadrant pain and can be performed simultaneously with a pelvic scan to look for a cyst or ectopic pregnancy.
- Probe Selection: In most patients, use a 5-7.5 mHz linear array small parts probe. For deeper imaging, you may need to obtain images with the 3-5 mHz curvilinear probe in patients with increased subcutaneous fat, or those in whom a retrocecal appendix is suspected.
- Technique Tips: Allow the patient to direct the ultrasound probe to the point of maximal tenderness. Begin imaging there. Look for a non-compressible round structure about 1cm in diameter. Always image in at least two planes: once you find a cross-sectional view of what appears to be an inflamed appendix, adjust your probe to look for a long-axis view. Confirm that the structure has a blind-tip at one end to avoid confusion with vascular or other structures.
- Diagnostic Criteria: Diagnostic criteria for acute appendicitis are as follows:
- A non-compressible, aperistaltic, tubular structure
- Diameter >7mm
- Blind-ended and connects to the cecum
- Other Signs:
- The “target sign” of inflamed muscularis propria surrounded by edema
- periappendiceal fluid
- prominent pericecal fat with stranding
- hyperechoic appendicolith within the tubular appendix
- presence of an abscess or phlegmon
- Negative Studies: You or your friendly sonographer must visualize a normal, compressible appendix on ultrasound to definitively rule-out appendicitis. Unlike with CT scan, this is rarely the case. If the appendix is not seen on ultrasound, you have a non-diagnostic study, so consider an 8 hour return visit for ongoing pain, a surgical consultation, or a CT scan
- Know Thy Surgeon: Not all surgeons are comfortable going to the OR based on an ultrasound that is positive for appendicitis. If the pretest probability is not already very high, your surgical colleagues may still request a CT scan. Don’t let that prevent you from doing the right thing for your patient. If you do more ultrasounds you &/or your ultrasound techs will become more proficient and your surgeons will eventually get more comfortable when repeated ultrasounds are confirmed by either CT or operative findings. If you impress your surgeons, they may even want to start borrowing your machine to do their own ultrasounds.
- Disadvantages: Ultrasound is far less likely to accurately identify other causes of right lower quadrant pain such as a kidney stone, Crohn’s disease, right sided diverticulitis, mesenteric adenitis and the like. Keep this and your differential diagnosis and relative levels of suspicion in mind when choosing your initial imaging study.
****
Usually it’s difficult to find a normal appendix with ultrasound.
Sometimes you get lucky.
Click below to see a brief video.
Click & Watch: Normal Appendix Peristalsing
****
****
****
INTUSSUSCEPTION PEARLS & PITFALLS:
- Scan the sausage: The intussusception usually sits in the right upper quadrant. If you feel something that is shaped like a sausage, that’s the best place to start your scan. You are looking for a “target sign” or “donut sign” of one concentric cross section of bowel within another.
- Know the pros and cons: Ultrasound has a reported sensitivity of 85% and specificity of 98% for intussusception and is radiation-free. However, it is not therapeutic. Since it is a rare condition, the skill level and experience of the sonographer may play a large role.
- Know your other studies: X-ray is not sensitive, but may show obstruction or decreased stool or air in the right lower quadrant. A CT scan can diagnose intussusception, but is not a first line study; consider its use when other conditions, such as appendicitis, are also high on your list of differential diagnoses. The study of choice is an air or gastrografin enema, which is diagnostic as well as therapeutic in most cases.
- Heed Pregerson’s Rule: This rule boils down to not trusting the consultant when your gut tells you they are wrong. It states “When the consultants says there is no way that a patient has disease-X the risk for disease-X doubles.” Corollary: “If the consultant is an orthopedist or a radiologist the risk quadruples.”
Intussusception with “Target” sign
****
Diagnosis of intussusception by physician novice sonographers in the emergency department.
Ann Emerg Med. 2012; 60(3):264-8 (ISSN: 1097-6760)
Riera A; Hsiao AL; Langhan ML; Goodman TR; Chen L Department of Pediatrics, Section of Emergency Medicine, Yale University School of Medicine, New Haven, CT. STUDY OBJECTIVE: We investigate the performance characteristics of bedside emergency department (ED) ultrasonography by nonradiologist physician sonographers in the diagnosis of ileocolic intussusception in children. METHODS: This was a prospective, observational study conducted in a pediatric ED of an urban tertiary care children’s hospital. Pediatric emergency physicians with no experience in bowel ultrasonography underwent a focused 1-hour training session conducted by a pediatric radiologist. The session included a didactic component on sonographic appearances of ileocolic intussusception, review of images with positive and negative results for intussusceptions, and a hands-on component with a live child model. On completion of the training, a prospective convenience sample study was performed. Children were enrolled if they were to undergo diagnostic radiology ultrasonography for suspected intussusception. Bedside ultrasonography by trained pediatric emergency physicians was performed and interpreted as either positive or negative for ileocolic intussusception. Ultrasonographic studies were then performed by diagnostic radiologists, and their results were used as the reference standard. Test characteristics (sensitivity, specificity, positive and negative predictive values) and likelihood ratios were calculated. RESULTS: Six pediatric emergency physicians completed the training and performed the bedside studies. Eighty-two patients were enrolled. The median age was 25 months (range 3 to 127 months). Thirteen patients (16%) received a diagnosis of ileocolic intussusception by diagnostic radiology. Bedside ultrasonography had a sensitivity of 85% (95% confidence interval [CI] 54% to 97%), specificity of 97% (95% CI 89% to 99%), positive predictive value of 85% (95% CI 54% to 97%), and negative predictive value of 97% (95% CI 89% to 99%). A positive bedside ultrasonographic result had a likelihood ratio of 29 (95% CI 7.3 to 117), and a negative bedside ultrasonographic result had a likelihood ratio of 0.16 (95% CI 0.04 to 0.57). CONCLUSION: With limited and focused training, pediatric emergency physicians can accurately diagnose ileocolic intussusception in children by using bedside ultrasonography.
****
WOULD YOU LIKE TO USE ONE OF OUR IMAGES?
As long as you paste the following statement with a weblink to this site, no problem: “Image reproduced with permission, ERPocketBooks.com”