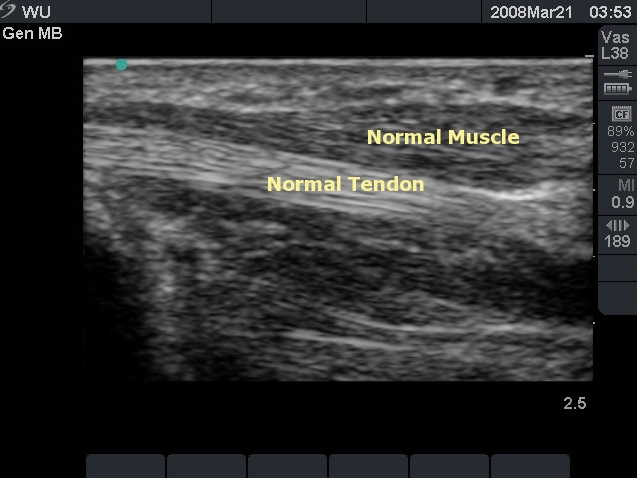
Normal Skin, Muscle and Tendon in the Hand
****
This webpage contains:
-
Cellulitis/Abscess/Nec-Fasc
-
Skin Foreign Bodies
-
Joint Effusions
-
Tendon Injuries
-
Nerves
****
Skin Ultrasound: Cellulitis, Abscess, or Nec Fasc?
- Probe & Positioning: Use a high frequency linear array transducer (10-13 MHz) for superficial structures and scans, such as soft tissue masses, in order to get more detail. Apply a large amount of ultrasound gel to improve your acoustic interface. For very superficial structures use a stand-off pad (you can improvise with a bag of saline) or, if feasible, water immersion.
- Target Confirmation: To avoid a case of mistaken identity, always obtain images in multiple planes (longitudinal, transverse, oblique). This helps determine if a structure is spherical or elliptical like an abscess, tubular like a vessel or elongated like a tendon or nerve. In addition, always utilize a contralateral side for comparison whenever possible.
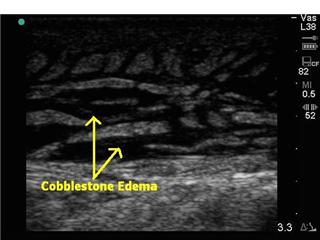
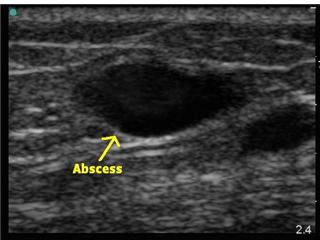
- Cellulitis or Abscess? Ultrasound can be used to help delineate whether a patient has cellulitis alone or a concomitant underlying abscess and to identify the size and depth of any fluid collection. Start by scanning normal tissue margins surrounding the area of interest. Normal subcutaneous tissue will have dark, hypoechoic regions of fat mixed in with brightly hyperechoic muscle, facial, and tendon planes. Cellulitis will demonstrate cobblestone edema. An abscess will show a spherical or elliptical collection of hypoechoic or heterogeneous material. While scanning, also try to identify nearby nerves, blood vessels and other structures to help prevent accidental damage during any planned procedure.
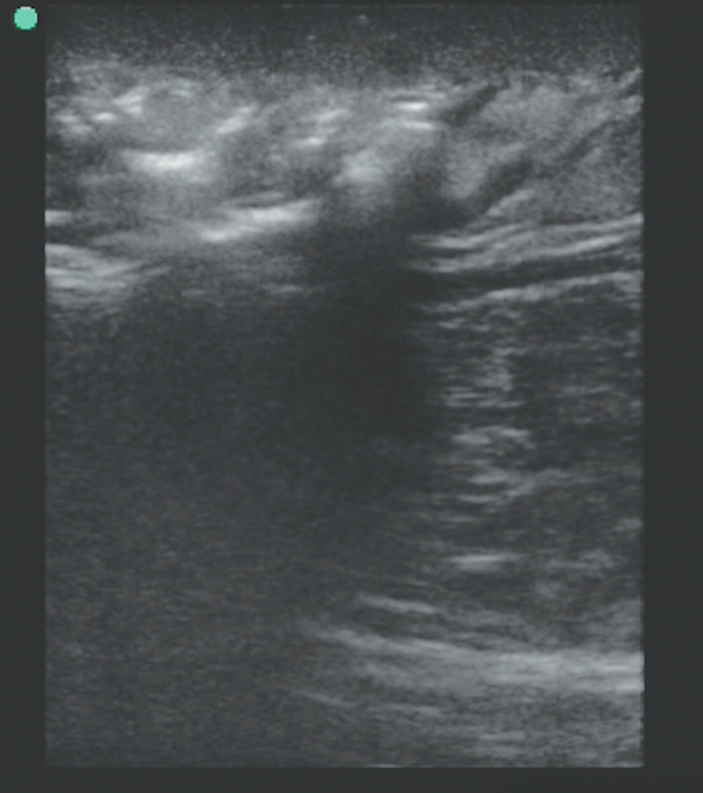
- Necrotizing Fasciitis: One should always consider the worst possibility in an ED patient. For soft tissue infections this would be Nec-fasc and ultrasound may be able to help at the bedside by identifying gas formation. Since pockets of gas reflect sound waves they appear hyperechoic. They also can cause dirty acoustic posterior shadowing and far-field reverberation artifact. During your scan be on the lookout for these findings within the skin and underlying tissue and fascia.
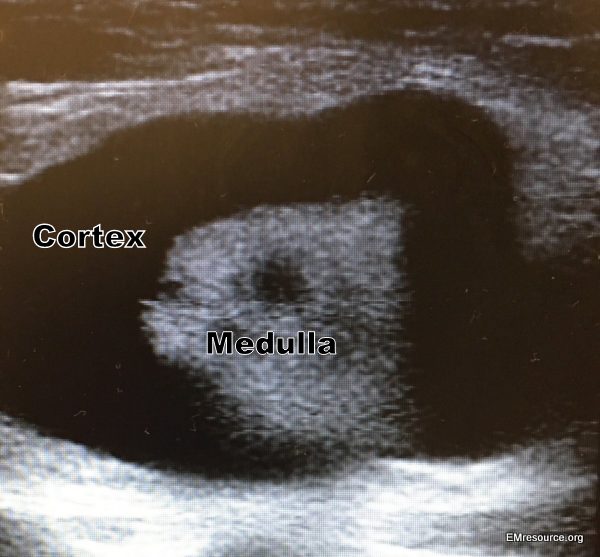
- Abscess Mimics: Pseudoaneurysms and large vessels may look like a fluid filled abscess on ultrasound. If you image in multiple planes, a vessel will appear as a cylinder but an abscess will remain egg-shaped. When in doubt, apply color-Doppler to the area of concern. Swollen lymph nodes can also mimic an abscess but usually have a hyperechoic central medulla and a hypoechoic outer cortex.
Cellulitis by soft tissue ultrasound. Courtesy of Teresa Wu, MD
****
Abscess by soft tissue ultrasound. Courtesy of Teresa Wu, MD
****
Necrotizing Fasciitis: Air is white with shadowing
****
Swollen Lymph Node
****
Foreign Body Ultrasound:
- Probe & Positioning: Use a high frequency linear array transducer (10-13 MHz) for superficial structures and scans. For very superficial structures use a stand-off pad (you can improvise with a bag of saline) or a water immersion.
- Target Confirmation: Obtain images in multiple planes (longitudinal, transverse, oblique) and utilize the contralateral side for comparison if necessary for clarification.
- Sensitivities: Know the Sensitivity of X-ray (XR) and Ultrasound (US) for different types of foreign bodies. Basically, x-ray is about 98% for gravel, metal and glass but almost useless for plastic and organic material. X-ray can also not be used real-time at the bedside to help localize. Ultrasound is about 30-50% sensitive for various types of foreign bodies. They will appear hyperechoic to different degrees and depending on material may produce different artifacts such as reverb, shadowing or even enhancement (glass). Sensitivity is lower for smaller objects like a cactus spine and also may lose sensitivity for organic material as time goes on and water is absorbed into the material. Below are some sensitivities for the study cited in the reference section
- Gravel: XR: ~98%, US: ~40%: hyperechoic with shadowing
- Metal: XR: ~98%, US: ~45%: reverberation or comet tail artifact
- Glass: XR: ~98%, US: ~50%: posterior enhancement rather than shadowing
- Cactus: XR: ~0%, US: ~30%: sensitivity likely low due to small size
- Wood: XR: ~0%, US: ~50%: sensitivity worse with time (absorbs water)
- Plastic: XR: ~0%, US: ~40%: probably not a common scenario
Glass FB with water immersion
****
Same patient: Glass FB WITHOUT water immersion and pressure on granuloma
****
Splinter – Wood is White
****
Splinter – Wood is White. Surrounding edema is dark
****
Find the Bullet Challenge
(answer way below)
****
Joint Ultrasound
- Look before You Leap: Ultrasound can be used to help you delineate whether a patient has a joint effusion or not. It is more sensitive than x-ray and can also help you localize the best area to tap. It may be prudent to perform a bedside ultrasound prior to an arthrocentesis attempt when physical exam findings are equivocal.
- Go Linear: For most joints use a 5 to 7.5 MHz linear array transducer. Apply a large amount of ultrasound gel to improve your acoustic interface. If the patient is thin and devoid of much subcutaneous fat, you may need to utilize an acoustic standoff pad or water submersion to improve your sonographic window.
- Take Multiple Views: Always obtain images in multiple planes (longitudinal, transverse, oblique) to help define the borders of the structure you are looking at and avoid mistaking vascular structures for a joint effusion.
- Compare Sides: Utilize contra-lateral limbs for comparison views, especially when unsure of what you see. If you see a similar structure on the asymptomatic limb, you may need to look again.
- Don’t Move: Avoid changing the position of the joint between performing the bedside ultrasound and performing the arthrocentesis. Fluid may move with joint repositioning.
- Practice Makes Perfect: With bedside ultrasound there is no substitute for experience. The more ultrasounds you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is.
Hip Effusion and Normal Comparison
****
Peripheral Nerves Ultrasound
- Probe & Positioning: Use a high frequency linear array transducer (10-13 MHz). Apply a large amount of ultrasound gel to improve your acoustic interface.
- Target Confirmation: Obtain images in multiple planes (longitudinal, transverse, oblique) and utilize the contralateral side for comparison when available.
- Arteries: are circular on cross section and difficult to compress. Color flow or Doppler can help confirm pulsatile flow
- Veins: are oblong or circular on cross section and easy to compress unless there is a DVT or they are obstructed. Color flow or Doppler can help confirm slow, steady flow.
Bones: Have a hyperechoic outer service with dense shadowing - Nerves: In cross sections nerves usually are described as having the appearance of honeycomb or a cluster of grapes.
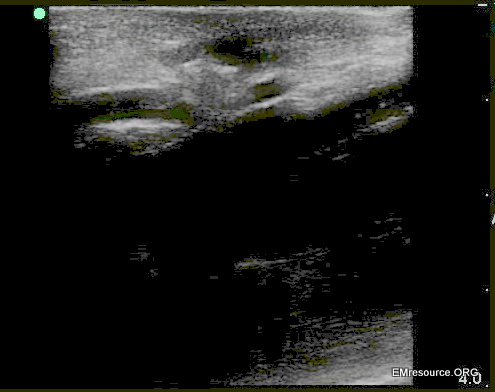
****
Structures of the Volar Wrist
****
Ulnar Nerve at Elbow
****
Tendon Ultrasound
- Probe & Positioning: Use a high frequency linear array transducer (10-13 MHz). Apply a large amount of ultrasound gel to improve your acoustic interface. For very superficial structures use a stand-off pad, such as a bag of saline, or if practical, employ water immersion for even better images.
- Target Confirmation: Obtain images in multiple planes (longitudinal, transverse, oblique) and utilize the contra-lateral side for comparison when available.
- Bones: Bones have a hyperechoic outer service with hypoechoic posterior shadowing. Ultrasound can be used to identify fractures x-ray is delayed or unavailable.
- Muscle: Skeletal muscle will appear hypoechoic with interwoven echogenic striations and hyperechoic fascial planes. Muscle tears and intramuscular hematomas can be identified by ultrasound.
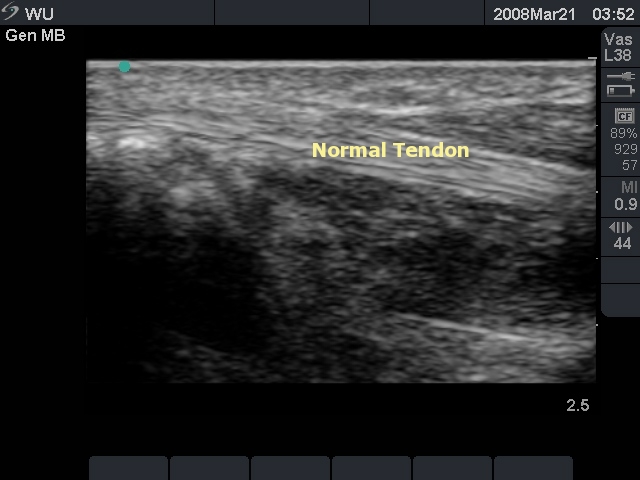
- Tendon Injury: Tendons appear brightly hyperechoic with visible linear fibers on long-axis scanning. Remember that normal function can be seen on physical exam with 90% tendon disruption. Partial or small tears can be assessed via bedside ultrasonography. Any hypoechoic or anechoic interruption in the hyperechoic tendon fibers should raise the suspicion of a tendon disruption. Subtle tendon damage may display an increase in the tendon cross-sectional area due to localized edema in the absence of actual tearing of the tendon fibers. Compare the area of interest to adjacent segments. If the ultrasound beam is not aimed directly parallel to the tendon fibers, a false hypoechogenicity artifact may be noted (anisotropy).
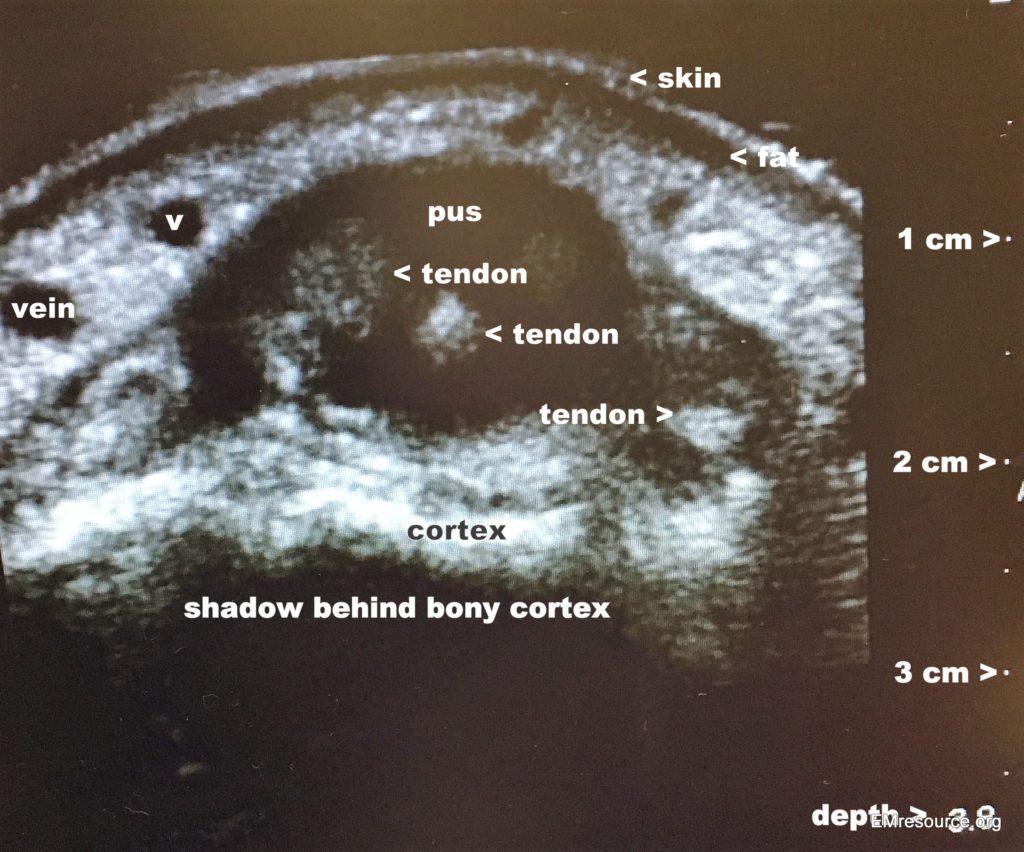
- Tenosyovitis: Fluid surrounding tendons will appear anechoic or hypoechoic and may signify infection or gout. It can also show tendonous attenuation from a destructive infection. If infection is suspected, immediate surgical drainage is usually indicated.

Septic extensor tenosynotivis: v = vein, T = Tendon
****
Same patient more proximally, near wrist
****
Normal extensor tendons of the hand
****
Normal Tendon: Flexor Pollicis Longus (Courtesy Teresa Wu, MD)
****
Normal Tendon: Flexor Pollicis Longus (Courtesy Teresa Wu, MD)
****
Lacerated Tendon: (Courtesy Teresa Wu, MD)
****
Gout: halo of fluid around tendon in foot
****
Can’t get enough educational images?
Check out the ED Atlas on CD, Volume 1
Do you want a pocket reference that has essential material on ED Ultrasound as well as other imaging, labs, EKG’s, procedures, risk management and more?
Then get the Tarascon Emergency Department Quick Reference Guide
****
WOULD YOU LIKE TO USE ONE OF OUR IMAGES?
As long as you paste the following statement with a weblink to this site, no problem: “Image reproduced with permission, ERPocketBooks.com”
****
Here’s the Bullet
****